Nervensystem steckt im Kampf oder Flug fest: Den Überlebensmodus verstehen und zur Regulierung zurückkehren
Phasen anhaltenden Stresses können den Körper in den Überlebensmodus versetzen, einen Zustand, in dem Wachsamkeit zur Standardeinstellung wird und das Nervensystem Schwierigkeiten hat, zur Ruhe und Regulierung zurückzukehren. Wenn sich ein Nervensystem entwickelt, das im Kampf oder in der Flucht feststeckt, kann diese Reaktion über den Zeitraum der tatsächlichen Bedrohung hinaus anhalten. Während diese Reaktion kurzfristig schützend wirkt, sind moderne Stressfaktoren selten kurz oder werden klar gelöst. Dies kann dazu führen, dass das Nervensystem auch dann noch auf Kampf oder Flucht ausgerichtet bleibt, wenn keine unmittelbare Bedrohung besteht1,2.
Um zu verstehen, wie man den Überlebensmodus verlässt, muss man über die Denkweise oder Willenskraft hinaus auf die zugrunde liegende Physiologie des autonomen Nervensystems blicken. Dieser Artikel untersucht die Bedeutung des Kampf-oder-Flucht-Modus aus wissenschaftlicher Sicht, erklärt, warum das im Kampf-oder-Flucht-Modus steckengebliebene Nervensystem bestehen bleiben kann, und skizziert evidenzbasierte Ansätze, die die parasympathische Regulierung unterstützen, einschließlich Schall, Atmung, sensorische Hinweise und moderne Neuromodulation durch nicht-invasive, transkutane Stimulation des Nervus auricular vagus (taVNS)3,4.
Ein Nervensystem, das im Kampf oder Flug stecken bleibt, ist eine physiologische Reaktion und kein persönliches Versagen
Die Kampf-oder-Flucht-Reaktion wird durch den sympathischen Zweig des autonomen Nervensystems vermittelt, der automatische Körperfunktionen steuert, die ohne bewusste Kontrolle ablaufen. Wenn eine potenzielle Bedrohung erkannt wird, erhöht sympathische Aktivität die Herzfrequenz, leitet den Blutfluss zur Skelettmuskulatur um, schärft die Aufmerksamkeit und unterdrückt nicht wesentliche Prozesse wie die Verdauung⁵.
Bei gesunder Regulation folgt auf die sympathische Aktivierung eine Rückkehr zum Ausgangswert durch parasympathische Aktivität. Wiederholte oder ungelöste Stressfaktoren wie anhaltende kognitive Belastung, emotionale Belastung, Schlafstörungen, Krankheit oder Umweltinstabilität können jedoch verhindern, dass diese Erholungsphase vollständig in Gang kommt6,7. Mit der Zeit kann das Nervensystem seinen Ausgangswert in Richtung Wachsamkeit neu kalibrieren, was dazu führt, dass das Nervensystem im Kampf oder in der Flucht feststeckt.
In diesem Zusammenhang spiegelt das “Feststecken” eher ein Muster autonomen Ungleichgewichts als Schwäche oder mangelnde Widerstandsfähigkeit wider. Ein Nervensystem, das im Kampf oder in der Flucht feststeckt, stellt eher ein physiologisches Muster als ein persönliches Versagen dar8.
Sympathische und parasympathische Systeme: Gleichgewicht über Unterdrückung
Das autonome Nervensystem funktioniert über zwei voneinander abhängige Zweige:
- Das sympathische Nervensystem, das Mobilisierung, Wachsamkeit und Energieverbrauch unterstützt.
- Das parasympathische Nervensystem, das Ruhe, Verdauung, Herz-Kreislauf-Regulation, Immunsignalisierung und Erholung unterstützt9.
Eine gesunde Regulation hängt von der Fähigkeit des Nervensystems ab, sich flexibel zwischen diesen Zuständen zu bewegen, anstatt von einem solchen dominiert zu bleiben. Wenn die sympathische Aktivität über einen längeren Zeitraum erhöht bleibt, kann diese Flexibilität abnehmen, was es für das System schwieriger macht, die Aktivität herunterzuregulieren, selbst in Umgebungen, die nicht mehr bedrohlich sind10. Unter diesen Bedingungen kann ein Nervensystem, das im Kampf-oder-Flucht-Modus feststeckt, trotz der Umweltsicherheit bestehen bleiben.
In Forschungsumgebungen wird die autonome Flexibilität anhand mehrerer physiologischer Marker bewertet. Ein häufig verwendeter Indikator ist die Herzfrequenzvariabilität (HRV), die Schwankungen im Zeitintervall zwischen den Herzschlägen erfasst. Eine niedrigere HRV wird häufiger beobachtet, wenn ein Nervensystem, das im Kampf-oder-Flucht-Modus feststeckt, die autonome Anpassungsfähigkeit bei anhaltendem Stress, anhaltender Müdigkeit und schlechter Laune einschränkt11,12,13.
Allerdings stellt die HRV nur ein Fenster zur autonomen Funktion dar und wird typischerweise zusammen mit anderen Messungen interpretiert, darunter Atemmuster, Blutdruckregulierung und Baroreflexempfindlichkeit.
Der Vagusnerv und die parasympathische Regulierung
Im Mittelpunkt der parasympathischen Funktion steht der Vagusnerv, der längste Hirnnerv im Körper. Es überträgt sensorische Informationen von Organen wie Herz, Lunge und Darm zum Hirnstamm und spielt eine wichtige Rolle bei der Regulierung des Herz-Kreislauf-Rhythmus, der Atemmuster, der Entzündungssignalisierung und der Stressbewältigung¹⁴.
Eine verringerte Vagusaktivität wurde mit einer niedrigeren HRV und einer verminderten Fähigkeit in Verbindung gebracht, aus erhöhter Erregung herauszukommen. Wichtig ist, dass die vagale Signalübertragung weitgehend afferent ist, das heißt, sie überträgt Informationen vom Körper an das Gehirn und beeinflusst so, wie Sicherheit und Bedrohung auf physiologischer Ebene interpretiert werden15,16. Ein verringerter Vagustonus wird häufig in einem Nervensystem beobachtet, das im Kampf oder in der Flucht steckt.
Für Personen, die herausfinden möchten, wie sie aus einem Nervensystem herauskommen, das in Kampf oder Flucht feststeckt, sind Ansätze, die die Vagusbahnen unterstützen, daher zu einem Bereich von wachsendem wissenschaftlichem Interesse geworden17.
Warum der Überlebensmodus bestehen bleiben kann
Der Überlebensmodus entwickelt sich selten als Reaktion auf ein einzelnes Ereignis. Häufiger entsteht es allmählich durch die Anhäufung wiederholter Anforderungen an das Nervensystem, manchmal über Monate oder Jahre18. Diese allmähliche Anhäufung ist eher charakteristisch für ein Nervensystem, das in Kampf oder Flucht feststeckt, als für eine akute Stressreaktion.
Zu den häufigsten beitragenden Faktoren gehören:
• Längerer psychischer Stress ohne ausreichende Genesung
• Wiederholte Exposition gegenüber Unsicherheit oder mangelnder Vorhersehbarkeit
• Gestörte zirkadiane Rhythmen und Schlafunregelmäßigkeiten
• Körperliche Erkrankungen oder postvirale Stressfaktoren
• Reduzierte Exposition gegenüber Hinweisen im Zusammenhang mit Sicherheit und Ruhe19,20
In diesen Kontexten kann es sein, dass das Nervensystem der Wachsamkeit weiterhin Priorität einräumt, auch wenn äußere Bedingungen dies nicht mehr erfordern. Diese Persistenz spiegelt adaptives Lernen auf der Ebene des autonomen Systems wider und ist eher ein entscheidendes Merkmal eines Nervensystems, das in Kampf oder Flucht feststeckt, als in einer bewussten Entscheidung21.
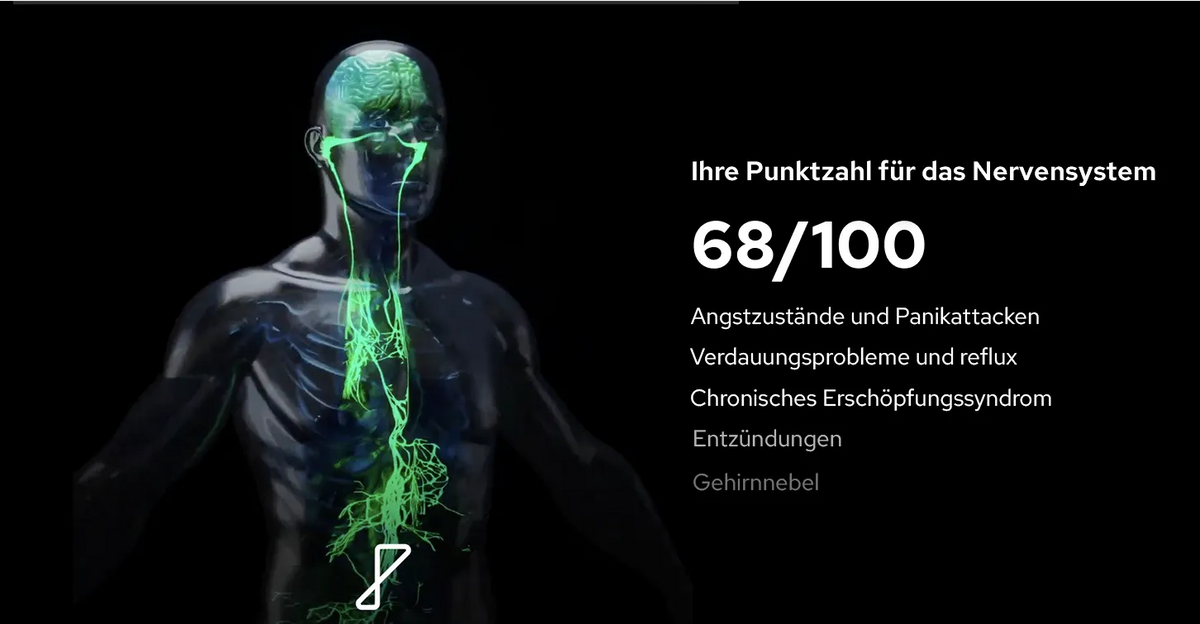
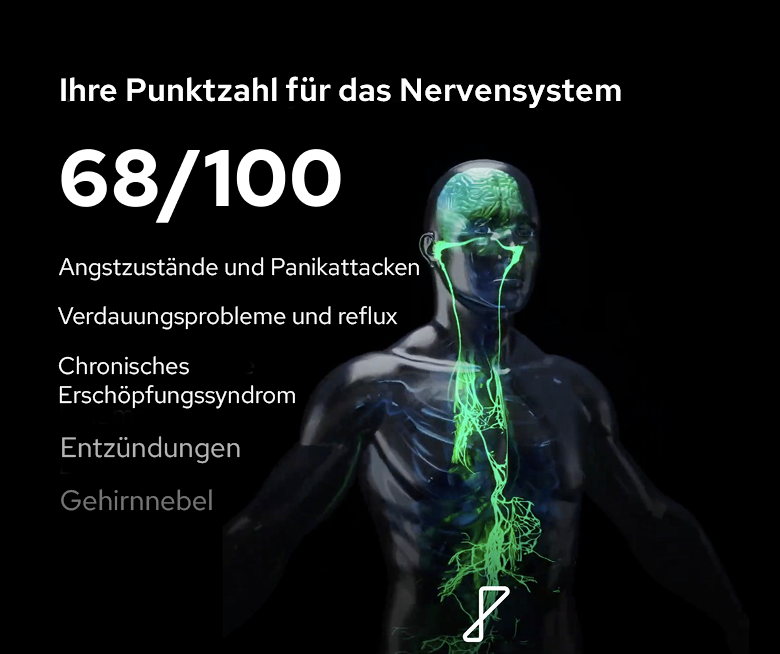
Abbildung: Eine längere Aktivierung des Nervensystems kann sich auf den gesamten Körper auswirken. Anstatt als einzelnes Symptom aufzutreten, manifestiert sich der Überlebensmodus häufig in emotionalen, kognitiven, physischen und verhaltensbezogenen Bereichen. In einigen Fällen kann dieser Zustand mit einem eingeklemmten Vagusnerv im Hals zusammenhängen, der ein Nervensystem widerspiegelt, das im Kampf oder in der Flucht feststeckt und auf Wachsamkeit und Schutz ausgerichtet bleibt, selbst wenn keine unmittelbaren Bedrohungen mehr bestehen.
Verlassen des Nervensystems, das im Kampf oder Flug feststeckt
Das Verlassen des Überlebensmodus erfolgt normalerweise nicht durch eine einzelne Aktion oder Technik. Stattdessen spiegelt es die kumulative Wirkung wiederholter Signale wider, die Sicherheit, Vorhersehbarkeit und Regulierung unterstützen —ein Prozess, der besonders relevant ist, wenn Symptome einer Vagusnervkompression in einem Nervensystem vorliegen, das in Kampf oder Flucht steckt.
Atmung und Rhythmus
Atmungsmuster beeinflussen direkt das autonome Gleichgewicht. Es wurde gezeigt, dass langsames, regelmäßiges Atmen sowohl bei gesunden Personen als auch bei klinischen Populationen parasympathische Marker verstärkt und die HRV verbessert22,23. Diese Effekte können einen stabilisierenden Input für ein Nervensystem liefern, das in Kampf oder Flucht steckt, sich allmählich entfaltet und eher auf Konsistenz als auf Intensität oder Anstrengung angewiesen ist.
Sensorische Eingabe und Ton
Das Nervensystem interpretiert kontinuierlich sensorische Informationen. Beruhigende, wenig erregende Höreingaben, die durch ein langsames Tempo, einen stabilen Rhythmus, minimale dynamische Variationen und begrenzte abrupte Änderungen gekennzeichnet sind – Merkmale, die häufig bei Ambient- oder Lo-Fi-Stilen zu finden sind – wurden daher als Mittel zur Reduzierung der sympathischen Hintergrundaktivierung untersucht. Dieser Ansatz kann insbesondere für ein Nervensystem hilfreich sein, das im Kampf oder in der Flucht feststeckt.
Untersuchungen deuten darauf hin, dass ein solcher auditiver Input kardiovaskuläre und respiratorische Parameter beeinflussen kann, die mit parasympathischer Aktivität verbunden sind24,25. Obwohl es sich bei Schall nicht um eine eigenständige Intervention handelt, kann er bei konsequenter und vorhersehbarer Verwendung zu einem allgemeinen Regulierungsumfeld beitragen26.
Bewegung und somatischer Input
Sanfte Bewegungen und berührungsbasierte Praktiken liefern sensorische Bottom-up-Inputs, die die autonome Regulierung unterstützen können. Ansätze wie langsames Yoga, intuitive Bewegungen, Dehnen oder Massagen führen Rhythmus und anhaltenden Druck ein – Reize, die mit einer leichten Verringerung sympathischer Marker und einer entsprechenden Erhöhung der parasympathischen Aktivität in Verbindung gebracht werden27,28. Diese vorhersehbaren, nicht bedrohlichen körperlichen Empfindungen können dazu beitragen, einem Nervensystem, das im Kampf oder in der Flucht feststeckt, Sicherheit zu signalisieren.
Ohrbahnen und Neuromodulation
Über verhaltensbezogene und sensorische Ansätze hinaus ist das Interesse an Methoden gewachsen, die die parasympathische Signalübertragung direkter unterstützen, insbesondere bei Personen mit einem Nervensystem, das in Kampf oder Flucht steckt. Der Ohrast des Vagusnervs bietet einen einzigartigen, nicht-invasiven Zugangspunkt zu vagalen afferenten Fasern am Außenohr. Diese Fasern projizieren in Hirnstammregionen, die an der autonomen Regulierung beteiligt sind, einschließlich des Nucleus tractus solitarius29,30.
Klinische Studien haben gezeigt, dass eine leichte elektrische Stimulation an dieser Stelle autonome Marker wie HRV und Baroreflexempfindlichkeit beeinflusst31,32. Dies hat zur Entwicklung tragbarer Systeme wie Nurosym geführt, die die parasympathische Signalübertragung durch nicht-invasive transkutane Stimulation des Nervus auricularis vagus (taVNS) unterstützen sollen, insbesondere dort, wo ein im Kampf-oder-Flucht-Modus steckengebliebenes Nervensystem ein anhaltendes autonomes Ungleichgewicht widerspiegelt.
Bei konsequenter Anwendung zielt dieser Ansatz darauf ab, die Fähigkeit des Nervensystems zu stärken, aus einer längeren Aktivierung auszusteigen, indem die an der physiologischen Regulierung beteiligten Wege unterstützt werden, anstatt Stressreaktionen in einem Nervensystem, das im Kampf oder in der Flucht feststeckt, vollständig zu unterdrücken.
Nurosym und parasympathische Unterstützung
Ein zertifiziertes, nicht-invasives tragbares System
Nurosym wurde von Parasym entwickelt und ist ein CE-zertifiziertes, nicht-invasives tragbares System zur Vagusnervenstimulation in der Europäischen Union, das entwickelt wurde, um etablierte Sicherheits- und Leistungsstandards für tragbare Geräte zur Vagusnervenstimulation zu erfüllen.
Nurosym kombiniert Stimulationsparameter, die mit denen in von Experten begutachteten Studien übereinstimmen, mit einem praktischen, ohrenbasierten Design für den täglichen Gebrauch. Im Gegensatz zu halsbasierten Systemen ist kein leitfähiges Gel erforderlich, was die tägliche Verwendung und den Transport vereinfacht. Die Stimulation bleibt auf sensorischem, schmerzfreiem Niveau und wird über den Ohrast des Vagusnervs abgegeben – ein Zugangspunkt, der in der autonomen Forschung umfassend untersucht wird33, insbesondere im Zusammenhang mit einem Nervensystem, das in Kampf oder Flucht feststeckt.
Präzisionskontrolle und alltägliche Benutzerfreundlichkeit
Ein Unterscheidungsmerkmal von Nurosym ist sein hoher Grad an Anwendungskontrolle. Das System bietet 45 einstellbare Intensitätsstufen, sodass der Vagusnervenstimulator an die individuelle Empfindlichkeit und die sich im Laufe der Zeit ändernden Bedürfnisse angepasst werden kann, einschließlich derjenigen, die mit einem Nervensystem verbunden sind, das im Kampf oder in der Flucht feststeckt
Die Sitzungsdauer kann von kürzeren Sitzungen an längere oder kontinuierliche Stimulation angepasst werden, was eine flexible Nutzung über verschiedene Routinen und Regulierungsstrategien hinweg unterstützt. Dieses Maß an Anpassungsfähigkeit ermöglicht den konservativen Einsatz des Systems bei niedrigen Intensitäten oder einen dauerhafteren Einsatz als Teil einer strukturierten autonomen Unterstützungsroutine für Personen mit einem Nervensystem, das in Kampf oder Flucht steckt.
Beweise im Einklang mit der autonomen Regulierung
In klinischen Studien zur transkutanen Vagusstimulation der Ohrmuschel wurden Protokolle, die auf die Parameter von Nurosym abgestimmt waren, mit messbaren Veränderungen physiologischer Marker in Verbindung gebracht, neben Veränderungen der gedrückten Stimmung, Angstzuständen, der Schwere der Müdigkeit, der Schlafqualitätswerte, der kognitiven Leistung und Entzündungsmarkern, die mit einem autonomen Ungleichgewicht in Zusammenhang stehen31,32,33,34,35,36 – Muster, die häufig in einem Nervensystem beobachtet werden, das in Kampf oder Flucht feststeckt.
61 % Steigerung der Vagusaktivität, 48 % Verringerung der Müdigkeit und 31 % Verbesserung der Schlafqualität
In relevanten erwachsenen Studienpopulationen wurde in unabhängigen Untersuchungen über messbare Veränderungen bei mehreren autonomen und erholungsbezogenen Ergebnismessungen nach Stimulation des aurikulären transkutanen Vagusnervs mit Nurosym berichtet. Hierzu zählen Erhöhungen der mit der Vagusaktivität verbundenen Marker um bis zu etwa 61 %, Verringerungen der ermüdungsbedingten Werte um bis zu etwa 48 % und Verbesserungen der Schlafqualitätswerte um bis zu etwa 31 %, wobei die beobachteten Effekte je nach Kohortenmerkmalen, Ergebnisdefinition und Stimulationsprotokoll variieren32,33,34,35,36.
45 % Verbesserung der stimmungsbezogenen Ergebnisse und 35 % Reduzierung ängstlicher Gedanken
Zusätzlich zu den physiologischen Effekten wurde in klinischen Studien eine Verbesserung der stimmungsbezogenen Ergebnismessungen um bis zu etwa 45 % sowie eine Verringerung der ängstlichen Denkmuster um bis zu etwa 35 % festgestellt. Diese Veränderungen stehen eher im Einklang mit einer verbesserten autonomen Regulierung und Flexibilität des Nervensystems als mit einer direkten Stimmungsänderung35,36.
Diese Erkenntnisse stammen aus einer wachsenden Zahl von von Experten begutachteten Forschungsarbeiten, die von unabhängigen akademischen und klinischen Gruppen in ganz Europa und den Vereinigten Staaten durchgeführt werden. Diese umfassen mehr als 50 abgeschlossene Studien, die sich mit physiologischen Merkmalen befassen, die für ein Nervensystem relevant sind, das in Kampf oder Flucht feststeckt.

Abbildung: Gemessene Verringerung der angstbezogenen Werte nach der Anwendung von Nurosym, ermittelt durch das Burns Anxiety Inventory. Das Bild zeigt einen signifikanten Rückgang vom Ausgangswert bis nach der Intervention, wobei die niedrigeren Werte bei der Nachuntersuchung erhalten blieben. Dies spiegelt wider, wie eine gezielte, nicht-invasive Stimulation des Vagusnervs mit Nurosym dazu beitragen kann, die Stressregulierung und Angstresistenz im Laufe der Zeit bei Personen zu unterstützen, deren Nervensystem in Kampf oder Flucht feststeckt.
Sicherheit, Maßstab und Einsatz in der realen Welt
Nurosym wurde in realen Umgebungen verwendet und weltweit wurden mehr als 4 Millionen Benutzersitzungen abgeschlossen. Diese Breite der Nutzung trägt zu einer wachsenden Evidenzbasis zu Sicherheit, Verträglichkeit und langfristiger Benutzerfreundlichkeit in verschiedenen Benutzerprofilen bei31,34, einschließlich derjenigen, deren Nervensystem im Kampf oder in der Flucht feststeckt.
Im Rahmen eines breiteren, auf Regulierung ausgerichteten Ansatzes wird Nurosym als Instrument erforscht, das dazu beitragen kann, die Fähigkeit des Nervensystems zu unterstützen, in einem Nervensystem, das in Kampf oder Flucht feststeckt, von einer längeren sympathischen Aktivierung weg und hin zu einer adaptiveren parasympathischen Regulierung überzugehen, insbesondere wenn es konsequent und zusammen mit anderen unterstützenden Strategien eingesetzt wird.
Wie Regulierung in der Praxis typischerweise aussieht
Das Verlassen des Überlebensmodus führt selten zu plötzlichen oder dramatischen Veränderungen. Häufiger erscheint die Regulierung als kleine, allmähliche Veränderungen in der Art und Weise, wie das Nervensystem auf alltägliche Anforderungen in einem Nervensystem reagiert, das im Kampf oder in der Flucht feststeckt. Dazu können gehören:
-
Einfachere Übergänge in die Ruhe
-
Reduzierte Grundspannung
-
Verbesserte Toleranz gegenüber alltäglichen Stressfaktoren
-
Stabilere Schlaf-Wach-Rhythmen
Wichtig ist, dass Regulierung nicht die Abwesenheit von Stress bedeutet, sondern eine erhöhte Fähigkeit, sich von der Aktivierung zu erholen und zum Gleichgewicht in einem Nervensystem zurückzukehren, das im Kampf oder in der Flucht feststeckt.
Neugestaltung des Überlebensmodus
Der Überlebensmodus spiegelt ein Nervensystem wider, das dem Schutz als Reaktion auf eine anhaltende Nachfrage Priorität einräumt. Aus physiologischer Sicht ist ein Nervensystem, das im Kampf oder in der Flucht feststeckt, weder ein Versagen noch ein fester Zustand, sondern ein adaptives Muster, das sich im Laufe der Zeit herausgebildet hat. Der Ausstieg aus dem Überlebensmodus hängt daher von wiederholten Signalen ab, die die Regulierung unterstützen, und nicht von Versuchen, Stressreaktionen zu unterdrücken.
Ansätze, die Vorhersehbarkeit und Konsistenz betonen, wie Atmung, sensorische Eingaben, sanfte Bewegungen und die Aktivierung parasympathischer Bahnen, stimmen eng mit der Anpassung des autonomen Nervensystems überein. Tools wie Nurosym, die die parasympathische Signalübertragung durch nicht-invasive transkutane Stimulation des Nervus auricularis vagus (taVNS) unterstützen sollen, bieten eine praktische Möglichkeit, die Regulierung des Nervensystems im Alltag für Personen zu stärken, deren Nervensystem in Kampf oder Flucht steckt
Durch diese Neugestaltung des Überlebensmodus verlagert sich der Fokus weg vom Nervensystem “der Fixierung” und hin zur Arbeit mit seinem zugrunde liegenden Design, was eine schrittweise Rückkehr zur autonomen Flexibilität im Laufe der Zeit unterstützt.
*Prozentuale Veränderungen spiegeln studienspezifische Ergebnismaße wider und sind kein Hinweis auf individuelle Ergebnisse.
Referenzen
-
McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87(3):873–904.
-
Herman JP, McKlveen JM, Ghosal S, et al. Regulation of the hypothalamic-pituitary-adrenocortical stress response. Compr Physiol. 2016;6(2):603–621.
-
Thayer JF, Lane RD. Claude Bernard and the heart–brain connection: further elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev. 2009;33(2):81–88.
-
Farmer AD, Strzelczyk A, Finisguerra A, et al. International consensus based review and recommendations for minimum reporting standards in research on transcutaneous vagus nerve stimulation. Front Hum Neurosci. 2020;14:568051.
-
Cannon WB. The wisdom of the body. New York: W.W. Norton & Company; 1932.
-
Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35(1):2–16.
-
Slavich GM. Social safety theory: a biologically based evolutionary perspective on life stress, health, and behavior. Annu Rev Clin Psychol. 2020;16:265–295.
-
Porges SW. The polyvagal perspective. Biol Psychol. 2007;74(2):116–143.
-
Floras JS, Ponikowski P. The sympathetic/parasympathetic imbalance in heart failure with reduced ejection fraction. Eur Heart J. 2015;36(30):1974–1982.
-
Thayer JF, Yamamoto SS, Brosschot JF. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Psychophysiol. 2010;74(2):95–101.
-
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93(5):1043–1065.
-
Bernardi L, De Barbieri G, Rosengård-Bärlund M, et al. New method to measure and improve consistency of baroreflex sensitivity values. Clin Auton Res. 2010;20(6):353–361.
-
Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms. Front Psychol. 2017;8:213.
-
Breit S, Kupferberg A, Rogler G, Hasler G. Vagus nerve as modulator of the brain–gut axis in psychiatric and inflammatory disorders. Front Psychiatry. 2018;9:44.
-
Butt MF, Albusoda A, Farmer AD, Aziz Q. The anatomical basis for transcutaneous auricular vagus nerve stimulation. J Anat. 2020;236(4):588–611.
-
Frangos E, Ellrich J, Komisaruk BR. Non-invasive access to the vagus nerve central projections via electrical stimulation of the external ear: fMRI evidence in humans. Brain Stimul. 2015;8(3):624–636.
-
Giannoni A, Gentile F, Passino C. Bioelectronic medicine and its applications in cardiology. Eur Heart J. 2022;43(46):4453–4455.
-
McEwen BS, Akil H. Revisiting the stress concept: implications for affective disorders. J Neurosci. 2020;40(1):12–21.
-
Walker WH, Walton JC, DeVries AC, Nelson RJ. Circadian rhythm disruption and mental health. Nat Rev Neurosci. 2020;21(9):1–16.
-
Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder. Psychol Bull. 2014;140(3):774–815.
-
Sterling P, Eyer J. Allostasis: a new paradigm to explain arousal pathology. In: Fisher S, Reason J, editors. Handbook of life stress, cognition and health. New York: Wiley; 1988. p. 629–649.
-
Lehrer PM, Vaschillo E, Vaschillo B. Resonant frequency biofeedback training to increase cardiac variability. Appl Psychophysiol Biofeedback. 2003;28(1):97–109.
-
Zaccaro A, Piarulli A, Laurino M, et al. How breath-control can change your life: a systematic review on psycho-physiological correlates of slow breathing. Neurosci Biobehav Rev. 2018;95:582–593.
-
Bernardi L, Porta C, Sleight P. Cardiovascular, cerebrovascular, and respiratory changes induced by different types of music. Circulation. 2006;114(20):209–216.
-
Thoma MV, La Marca R, Brönnimann R, et al. The effect of music on the human stress response. PLoS One. 2013;8(8):e70156.
-
Koelsch S. Music-evoked emotions: principles, brain correlates, and implications for therapy. Brain Cogn. 2015;89:80–89.
-
Field T. Massage therapy research review. Complement Ther Clin Pract. 2016;24:19–31.
-
Streeter CC, Gerbarg PL, Saper RB, et al. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis. J Altern Complement Med. 2012;18(12):1145–1152.
-
Antonino D, Teixeira AL, Maia-Lopes PM, et al. Non-invasive vagus nerve stimulation acutely improves spontaneous cardiac baroreflex sensitivity. Brain Stimul. 2017;10(5):875–881.
-
Bretherton B, Atkinson L, Murray A, et al. Effects of transcutaneous vagus nerve stimulation in individuals aged 55 years or above. Aging (Albany NY). 2019;11(14):4836–4857.
-
Nagai M, Dote K, Kato M, et al. Blood pressure variability after non-invasive low-level tragus stimulation in acute heart failure. J Cardiovasc Transl Res. 2024;17(6):1347–1352.
-
Gentile F, Giannoni A, Navari A, et al. Acute right-sided transcutaneous vagus nerve stimulation improves cardio-vagal baroreflex gain in patients with chronic heart failure. Clin Auton Res. 2025;35(1):75–85.
-
Stavrakis S, Elkholey K, Morris L, et al. Neuromodulation of inflammation to treat heart failure with preserved ejection fraction. J Am Heart Assoc. 2022;11(10):e023582.
-
Dalle Luche G, Dundovic S, Stavrakis S, et al. First report of safety and tolerability of low-level tragus vagal neuromodulation in cardiovascular patients. J Am Coll Cardiol. 2024;83(13 Suppl A):178.
-
Zheng Z, et al. Transcutaneous vagus nerve stimulation improves Long COVID symptoms in a female cohort: a pilot study. Front Neurol. 2024.
-
Verbanck P, et al. Transcutaneous auricular vagus nerve stimulation (tVNS) can reverse the manifestations of the Long-COVID syndrome: a pilot study. Adv Neurol Neurosci Res. 2021.
Haftungsausschluss: Dieser Artikel dient nur zu Bildungszwecken und bietet keine medizinische Beratung. Nurosym dient nicht der Diagnose, Behandlung, Heilung oder Vorbeugung von Krankheiten. Konsultieren Sie für eine individuelle Beratung immer einen qualifizierten Arzt.